The following article provides background information about treating of kidney disease in Canada and Germany. Subject-matter experts of the NephroCAGE consortium share details of the disease’s complexity, dialysis and organ transplantation as therapy options as well as possible risks and side effects. The number of patients waiting for an organ donation exceeds organ donations by far. With an aging population this trend is expected to raise. Therefore, the risk of organ rejection or organ failure after transplantation will be of huge importance in future.
Thanks to the contributing experts from our partners for their input for this article: Dr. Matthieu-P. Schapranow (HPI), Dr. Ruth Sapir-Pichhadze (McGill), Dr. Marcel Naik (Charité), Aadil Rasheed (HPI). Photo by Robina Weermeijer.
Kidneys: What are these organs good for?
Typically, healthy people have a set of two working kidneys in their body. One of their important functions is to filter toxins and waste products and excrete excessive fluids from the blood stream. Moreover, kidneys play important role in bone health and blood pressure regulation by producing hormones and modifying vitamin D.
Kidney disease: A diagnosis with multiple facets
Kidney diseases are classified in two main categories: acute kidney disease (AKD) and chronic kidney disease (CKD). The acute form is often life-threatening and requires immediate action and intensive care. Whereas people suffering from the chronic form can live a normal live with minor limitations. Regular dialysis is one of the common treatments in patients with insufficient kidney function. Another treatment option is kidney transplantation. A kidney transplant costs around 15-20 thousand Euros, which is about half of the annual dialysis costs per patients. However, it is a long complex surgery requiring many medical experts from a transplant team but still has multiple risks. Also, donor organs are limited, required organs exceed available organs, and finding the best matching organ is a very complex task.
Situation in Canada and Germany
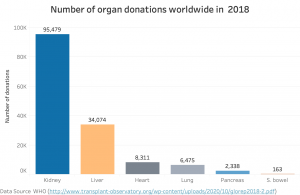
- Fig. 1: Comparison of worldwide donations by organ (2018)
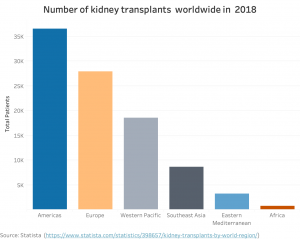
- Fig. 2: Number of performed kidney transplants by region (2018): America and Europe are leading regions with together more than 65k kidney transplants per years.
- Fig. 3: Number of patients on a waiting list for a kidney organ in Canada and Germany (2019)
- Fig. 4: Number of patients on a waiting list in Canada and Germany per 100k of population (2019): Canada and Germany have a very similar ratio of about 8.6-8.8 per 100k.
As shown in Figure 1, kidney is the number one donated organ worldwide. More than 95k kidney transplants in total were performed worldwide in 2018 as shown in Figure 2.
In Germany, there were about 100k patients on dialysis in 2019 and in Canada, there were about half as many. Out of those dialysis patients, there are 7k patients on the kidney transplantation waiting list in Germany and over 3k patients in Canada, as shown in Figure 3. However, people on waiting list per 100,000 people is in both nations comparable as depicted in Figure 4.
More than 1.9k kidney transplants were performed in Germany in 2020 according to German Organ Transplant Foundation [1] and almost 1.8k kidney transplantations in Canada in 2019 according to Canadian Institute for Health in Canada [2].
Eventual complications after kidney transplantation
Patients with kidney transplantation require constant follow-up care. Despite excellent short-term graft survival rates, long-term graft survival has remained unchanged with about five percent graft loss per year after the second year of transplantation. Reasons for graft loss are rejections, additional comorbidities, acute infections and drug toxicities.
Rejection in this context means that the immune system of the organ recipient begins to recognize the kidney tissue of the new organ as foreign tissue, creates antibodies against the Human Leukocyte Antigen (HLA), and starts to attack the implanted kidney. The absence of pre-formed antibodies does not protect patients from experiencing rejection, because patients can develop antibodies against the donor tissue after transplantation. This often happens when patients do not take their post-transplant medications as prescribed or because a doctor decreased the prescribed medications to deal with other complications, such as infections or medication side effects.
Best practices to prevent complications after kidney transplantation
To prevent rejection, patients receive a specific set of medications known as immunosuppressants, which prevent the recipient’s immune system from attacking the new kidney. However, medical professionals have to adapt the right dosage and optimal combination of medications for each individual patient over time.
Matching donors and recipients
Matching the donor’s and the recipient’s immune system with each other in advance can help to identify adequate peers, who will not develop antibodies. Historically, the three regions A, B and DR on the HLA gene are used for matching only. In Canada, Canadian Blood Services (blood.ca) in collaboration with various partners established The Highly Sensitized Patient (HSP) Program. It provides a set of software tools for Calculated Panel Reactive Antibodies (CPRA), which gives the theoretical incompatibility between deceased organ donors and the transplantation candidate. As a result, a high CPRA score indicates that the specific patient is incompatible with higher percentage of deceased donors. Therefore, the expected wait time for a compatible donor is higher for the given patient.
Innovative donor-recipient matching towards the no-rejection aim
Recent diagnostic advances and research findings brought up an even more advanced type of matching: epitope matching. Epitopes are specific parts of the antigen. Today, the complexity of the immune system makes epitope matching still very compute-intensive. However, experts believe that it might be even more relevant than genetic matching.
The NephroCAGE consortium
The German Canadian consortium NephroCAGE combines medical and scientific-technical expertise from Germany and Canada. We jointly create a learning clinical system that tests the added value of the latest artificial intelligence (AI) techniques on the concrete clinical example of kidney transplantation. Therefore, our NephroCAGE partners create a learning AI system that will be used to match organ donors and recipients even more precisely in advance in order to reduce risks in kidney transplants and prevent graft loss. To this end, clinical centers of excellence in both nations are contributing transplant data from the past 10 years. They will be analyzed using AI learning techniques and combined with a novel matching algorithm to create clinical prognostic models for kidney transplant recipients. NephroCAGE aims to support clinical workflows towards the goal of zero kidney transplant rejection using intelligent insight and next generation matching from examination reports of the patients.





Comments are closed